Making sense of treatment options for sleep apnea
- Posted on: Jun 20 2017
The diagnosis and treatment of sleep apnea remains one of the more complex algorithms in medical therapy. The ways to diagnose sleep apnea have been covered elsewhere in this blog well as other articles. We will focus on treatment options for this particular article.
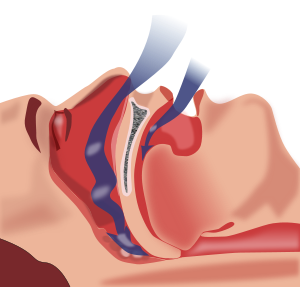
Before we discuss the treatment options, it is important to understand what is the overall aim of the treatment options. Sleep apnea is by definition a condition of inadequate airflow though the upper airway passages, particularly during sleep, which then leads to inadequate oxygenation and disturbed sleep. There is never strictly only one point within the upper airway that is responsible for all of any one person’s obstruction. Some of the obstruction is probably in the nostrils, some from the septum, some from possible polyps in the nose or adenoids in the back of the nose. Some of the obstruction could come from big tonsils, some from a long palate, and some of it from the tongue flopping back and blocking the throat. Additional blockage could also come from a narrow collapse of the throat walls as a function of breathing. Therefore, it is unrealistic to expect to fully correct the anatomical blockage at any one point and have the sleep apnea completely disappear. In order to make people understand this better, I usually like to compare what happens during sleep apnea to what happens if you have to drive your car from midtown to your home in the suburbs. Chances are you will hit some traffic on the main street. Perhaps some additional traffic getting onto a bridge. Even more traffic when you get on the highway. And then some bottlenecking traffic when you take the exit. Even if you do your best to completely fix any of the usual traffic spots, your overall traffic delay is the function of combining all the traffic spots and how they affect your commute home.
Although there are many types of treatments that we offer to patients, I personally like to put them into three general categories: Device therapy, surgery, and weight reduction.
DEVICE THERAPY: There are many devices designed to improve airflow in the upper airway in order to decrease the symptoms of sleep apnea. Generally, they fall within two categories: Passive and active.
Passive Devices: These devices are not powered, and are designed to provide static improvement for the air flow. They are usually applied right before going to bed, and are designed to keep the airway open throughout the night sleep. One of the more common devices that is easily obtained are the nasal strips. These adhere to the top of the nostrils, and by flaring them out allow more air in and out of the nose without much friction. Some people also use cones that go within the nostrils and achieve the same result internally. Alternatively, Provent® is a valve mechanism which is a disposable item. This allows unobstructed inspiration, but with sight resistant upon expiration in order to keep the airway open. Other devices include oral appliance that sits in the mouth and pushes the tongue and the jaw forward in order to prevent collapse into the back of the throat. With adequate use, these passive devices can provide a decent amount of relief for most patients. The significant drawback of any of the devices mentioned is that they usually work on only one part of the anatomy, not all of it. Unfortunately, most people suffering from sleep apnea have multiple points of obstruction, and might not respond to any one of these devices as optimally as needed.
Active Devices: Active devices usually include CPAP and BiPAP masks. These are powered devices that will try to coordinate with breathing in order to keep the airway open. Of all the possible treatment options, these active devices have the highest rate of success in alleviating the obstruction. Using the multiple points of traffic analogy from above, these devices “shoot” the air through all the traffic to make sure the oxygen reaches the very far reaches of the lung no matter how many points of blockage it encounters. Unfortunately, like all devices, they do not change the anatomy in a long-term, and the rate of success is very dependent on compliance and continued use after months and years.
SURGERY: Unlike devices, surgery could offer a one-time option of improving the anatomy so that the breathing is much more efficient and to avoid blockage issues related to obstructive sleep apnea. However, each kind of surgery focuses on one part of the anatomy. Many people might need to focus on surgery on multiple points within the anatomy to fully address all the obstructing areas.
Some of the more common types of surgery that are performed for sleep apnea are septoplasty to straighten out the midline wall of the nose, turbinate reduction to remove the bulkiness of the side walls of the inside of the nose, and polypectomy to reduce any obstructive lesions within the nasal passages.
Surgeries that would be performed within the mouth and the throat would include tonsillectomy to remove bulkiness within the throat, as well as uvulopalatopharyngoplasty to remove the excess tissue within the throat. More advanced procedures would include hyoid suspension, base of tongue reduction and maxillomandibular advancement protocols, which are typically more invasive.
WEIGHT REDUCTION: Optimizing the patient’s weight is one of the more important factors in correcting for sleep apnea. By definition, sleep apnea is a condition of inadequate supply of oxygen. Therefore, the more weight the patient has, the higher is the oxygen demand. Conversely, the lower the weight, the less oxygen the patient can do away with nicely. The second issue has to do with circumference of the neck. People with excess weight have bulkier necks which then in turn results in more narrow windpipes. If the weight is lost successfully, the windpipes can extend and actually accommodate more air exchange without much friction.
Many people may need to resort to one or more of the treatments described above to correct for sleep apnea problems. The outcome is quite diverse from one patient to the next. Ideally, each patient should have an individual consultation with their health care provider to see what line of therapy is best for them, and to make a decision appropriate to their own circumstances.
Tagged with: apnea, bipap, CPAP, ear nose throat, ENT, Isaac Namdar, Isaac Namdar MD, mandibular device, nasal strips, New York, new york city, night guard, ny, NYC, Otolaryngology, Otorhinolaryngology, provent, septoplasty, sleep apnea, snoring, Tonsillectomy, turbinate reduction, turbinates
Posted in: Sleep Apnea